Aneurysmal Bone Cyst (ABC) is a non malignant, tumour like vascular and reactive malformation comprised of blood filled channels
It is usually a single, expansive and aggressive lesion involving the bones.
Incidence
- 1-6 % of primary bone tumours
Age Predilection
- It is most commonly seen in the age group of 15-25 years.
- Rare in adults or elderly.
Location
- It is found in the metaphysis and epiphyseal of long bones (upper extremity and lower extremity)
- Pelvis, spine uncommon (large volume disease often)
What is the cause of Aneurysmal bone cyst?
- It is suspected to be related to trauma.
- It is also found as a secondary component of other tumors such as:
- Giant cell tumor
- Chondroblastoma
- Fibrous dysplasia
- Osteoblastoma
- Chondromyxoid Fibroma
- Osteosarcoma & Chondrosarcomas
- Genetic research: Specific translocations of the TRE17/USP6 gene [due to t(16,17) translocation and upregulation which halts osteoblastic maturation] are reported in about 70% of primary ABC but never in secondary ABC lesions.
- https://journals.sagepub.com/doi/full/10.1177/1066896920938878
How is ABC identified?
- Pain is commonest symptom. It is often dull aching.
- Swelling of several weeks duration.
- Pathological fracture (fracture of weakened bone due to trivial fall) is common due to aggressive nature.
- Occasionally, neurological symptoms if lesion is pressing on spinal cord
- https://bonecancer.in/2020/05/01/arriving-at-diagnosis-services/
Imaging
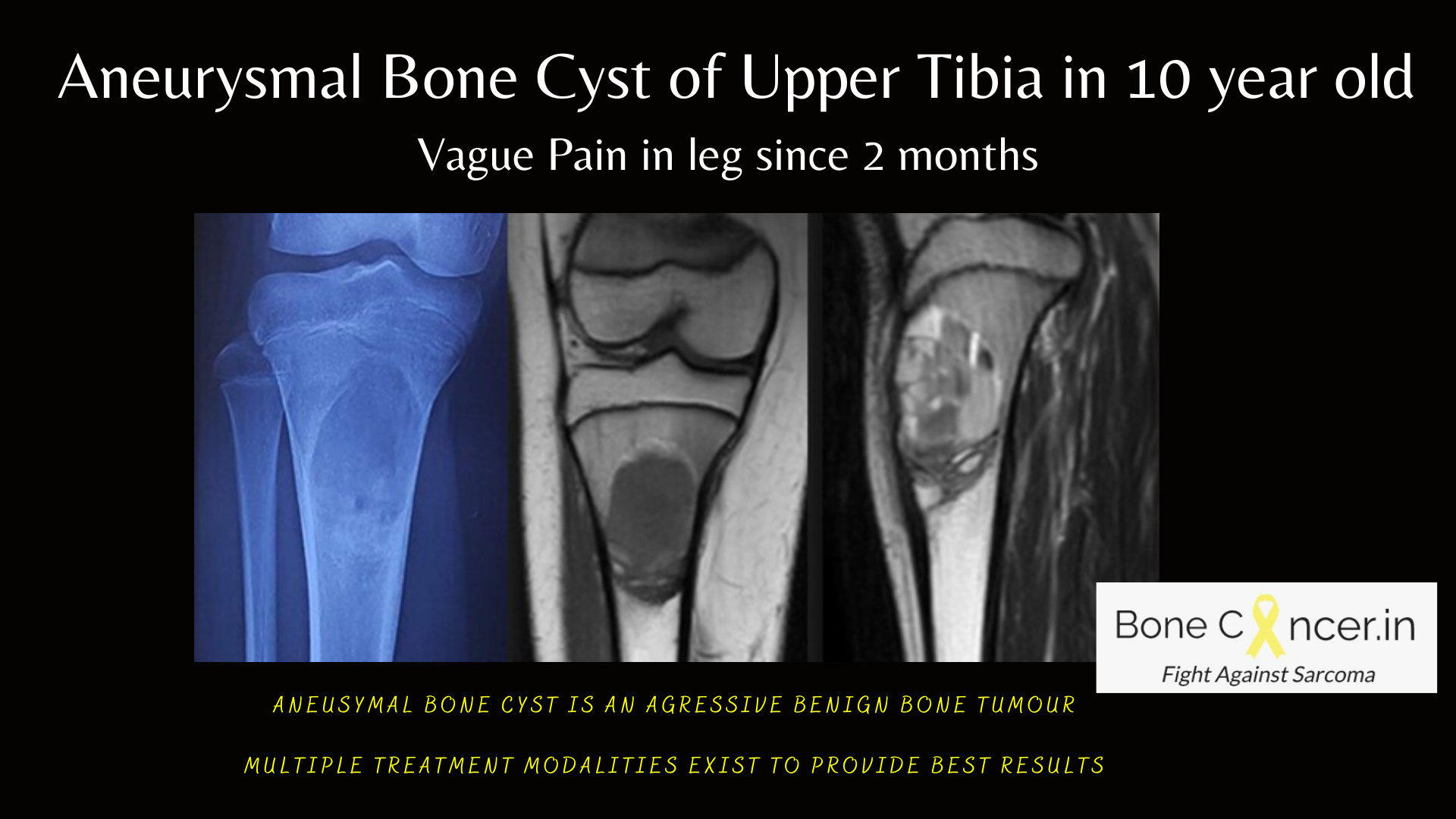
- Plain radiographs show a solitary, expanded cavity with cystic or osteolytic lesion, with thin “eggshell” sclerotic borders.
- The enclosed cavity contains many dividing septa with expanding soap bubble appearance.
- MRI is necessary to diagnose ABC, and the typical finding is Multiple Fluid-Fluid levels on T1 contrast and T2 weighted images.
- CT is not done often. May show egg-shell rim with fluid fluid levels with contrast
- Biopsy (Needle) is mandatory to diagnose ABC as it can mimic any of the other benign or even malignant bone tumors.
- Pathological examination shows blood filled cyst cavities with giant cells, spindle cells, fibroblasts without atypia.

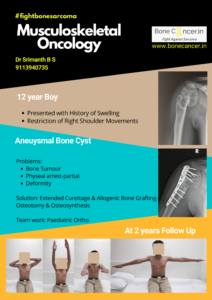
Aneurysmal Bone Cyst of Proximal Humerus with Deformity in a child.
How is ABC treated?
Treatment of ABC depends upon location and aggressiveness of lesions.
Very few ABC’s can be in latent or inactive stage, not needing any intervention.
Treatment options are as follows:
- Minimally Invasive- Image Guided
- Percutaneous curettage (Curopsy)
- Percutaneous Sclerotherapy (polidocanol, 3 % asklerol) under radiological guidance
- Usually needs to be repeated at 2-3 month intervals, with average healing time of 5 months.
- Surgery
- Extended Curettage to clear tumor followed by filling or reconstruction of the defect with bone grafts similar to GCT.
- Adjuvants can be used, but there is no clear evidence of benefit.

Aneurysmal bone cyst of proximal humerus with deformity treated by Extended Curettage, Allogenic Bone Graft & Plate Osteosynthesis
- Alternate Treatment Strategy OR Combination Strategy in Large Size OR Axial OR Inoperable Situations.
- Percutaneous Serial Arterial Embolization can be carried out with aid or Interventional Radiologist with good results to decrease the size of tumor.
- Recently, there has been a shift in treating ABC’s by minimally invasive surgical procedures like Curopsy and/or Sclerotherapy, due to similar results noted between surgical and minimally invasive procedures.
- In some situations, when the tumour has grown so large, resulting in pathological fracture or when the bone is not salvageable, a resection and reconstruction procedure (biological or Tumor endoprosthesis) is carried out.
Does ABC reappear?
- The recurrence rate in long bones after curettage alone is 20-35 % which can be reduced by performing extended curettage resulting in risk of local recurrence at 10%
- Similar rates of recurrence are being observed when ABC’s are being treated by Curopsy and/or Sclerotherapy.
- ABC is aggressive and may add to morbidity.
- It does not metastasize and is not fatal.
- Adjuvant treatment with Zoledronic acid or Denosumab is encouraging but has limited scientific data.


2 Comments