Giant Cell Tumour
Symptoms |Signs | Treatment Options
Giant cell tumor (GCT) of bone is an aggressive benign tumor.
Age Predilection
- Common age group is 20 – 40 years, more commonly in women.
Location
- GCT is Eccentric, Epiphyseal and Expansile involving Epiphysis part of bone.
- Seen commonly around the knee joint, distal radius, hip, shoulder and pelvis in decreasing frequency.
Etiology of GCT?
- Etiology is unknown.
- They appear to be an extensive proliferation of Osteoclasts (cells which are part of the remodeling process in bone), eating away the normal bone architecture.
- GCT can also rarely (2-5 %) metastasize to lungs, but is not fatal and treatable.
How is GCT identified?
- They can present as a small contained tumor or an aggressive type expanding the bone and producing a clinically noticeable swelling.
- Pain
- 3-6 months duration average
- Dull aching, associated or aggravated with movement.
- Swelling In the later stages as the tumor expands, pain is more.
- Pathological fracture if left untreated
- https://bonecancer.in/2020/05/01/arriving-at-diagnosis-services/
- https://bonecancer.in/2020/05/01/biopsy/
How is GCT Identified?
Imaging
- Plain radiograph shows eccentric lytic lesion placed in metaphysis-epiphysis area of long bone with varying destruction of surrounding bone.
- The tumor when aggressive or diagnosed in late stage may have soft tissue extension
- MRI shows T1 hypointense and T2 hyperintense lesion with solid component.
- Areas of fluid fluid levels may be seen (Secondary ABC Component)
- Image guided Core Needle
- Histopathological examination shows Stromal cells and ‘Multinucleated Giant cells’ in abundance.
What are the grades of GCT?
- GCT can be classified according to Campanacci Classification.
- Treatment may vary depending on the stage and location of GCT.
- Latent (Grade 1): Well defined, contained lesion with intact surrounding bone/cortex.
- Active (Grade 2): Relatively well defined but very thin surrounding bone or cortex.
- Aggressive (Grade 3): Indistinct borders, surrounding bone destruction and soft tissue component due to expansion.
How is GCT treated?
- Primary treatment is surgery- Extended Curettage https://bonecancer.in/2020/05/15/extended-curettage-2/
- Extended curettage is a procedure wherein the surgeon clears the cavity of the tumor by opening the capsule and extending the clearance with aid of high speed burr (1-2 mm).
- This ensures a thorough clearance or curettage or GCT and reduces the rate or tumor recurrence to 10%.
- Adjuvants such as Hydrogen Peroxide, Phenol or Liquid Nitrogen can also be used to help kill the tumor cells and reduce the recurrence rate locally, but the clinical evidence is not very strong to advocate its use.
- We currently use an Argon Laser beam to burn the wall of the cavity and have provided excellent results.
Reconstruction is done using the following alone or in combination
- Bone Grafts (Autograft)
- Bone Grafts (Allograft)
- Utilizing a bone graft provides a more ‘Native or Biological’ reconstruction helping the biomechanics of adjacent joint.
- Disadvantage is the time taken to heal or incorporate into native bone, until then the limb has to be protected.
- Cement (PMMA)
- Cement is utilized for filling the defect and provides immediate structural support.
- Several scientific studies suggest that cement usage may have the advantage of identifying a local recurrence early compared to bone graft.
- There is also concern of early osteoarthritis when used close to joint cartilage.

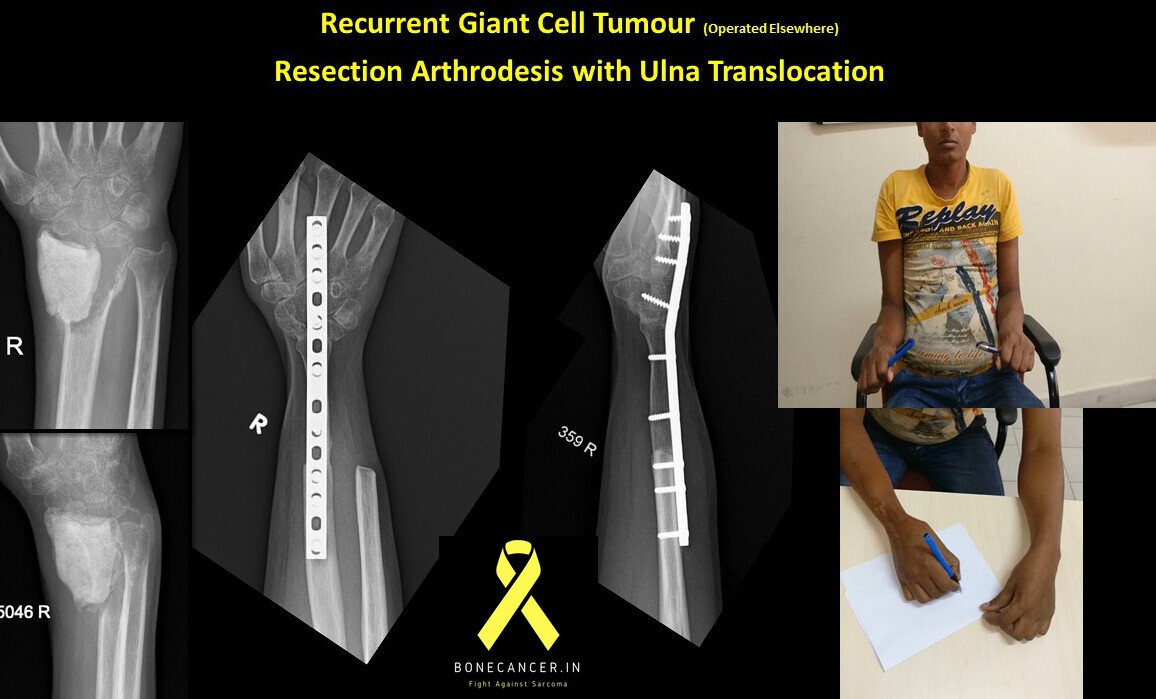
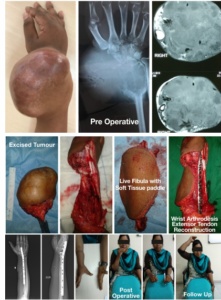
Giant cell tumour of Lower Radius: Limb Salvage surgery with tumour resection- wrist arthrodesis with Free Fibula
- Screws, Plates and/or nail with above fillers
- The choice of filling the defect is hence individualized based on many factors, especially the stage, location of tumor, proximity to adjacent joint and function it has to perform.
- En-Bloc Resection & Limb salvage surgery
- Rarely, a GCT which is Grade 3 or late presentation with adjacent joint destruction may require surgical removal of the tumor with capsule and soft tissue in toto.
- The defect can be reconstructed with various Limb Salvage options with tumor prosthesis, arthrodesis and biological reconstructions.

- Additional or Alternative treatments for GCT?
- GCT in certain areas such as Pelvis, Sacrum and Spine may not be suitable for primary surgical treatment always due to high morbidity.
- Following treatments may be used alone in in combination:
- Zoledronic acid (4 mg intravenous) has been reported to reduce local recurrence when used intra or pre operatively.
- A new drug, Denosumab is currently indicated for non operable GCT in axial skeleton or in downstaging the tumour to a resectable situation, thereby decreasing morbidity of treatment.
- Angioembolization, either pre surgery or as definitive treatment.
- May require it to be done single or in multiple settings.
- However, these drugs are not advocated for routine use in giant cell tumours and have to be used with caution with due consideration to benefits and risks involved.
Does GCT reappear?
- Local recurrence rate of GCT currently ranges between 4-18 %. in data worldwide.
- The use of High speed burr in extended Curettage reduces the risk of recurrence to between 4-8 % (with or without the usage of adjuvants).
- The Local recurrence when diagnosed can again be treated with extended curettage with excellent results.
- Rarely, a large or multiple local recurrence may need surgical excision and reconstruction by other methods.
- Radiotherapy is used sparingly in GCT due to risk of secondary sarcomatous changes.
What is the course of GCT?
- GCT is not fatal, even though reports of multiple synchronous occurrences or metastases to lungs have been reported.
- Lung metastases respond well to Zoledronic acid/Denosumab treatment and rarely need surgical removal.
- Aggressive monitoring is performed every 3 months for 2 years (Plain radiographs and Chest radiograph/CT of Chest) and thereafter annually.
For More Information CONTACT US

1 Comment